
- #Explain alphabetic index and tabular list quizlet full
- #Explain alphabetic index and tabular list quizlet code
If no bilateral code is provided and the condition is bilateral, assign separate codes for both the left and right side. An unspecified side code also is provided in instances where the side may be unidentified in the medical record.
#Explain alphabetic index and tabular list quizlet full
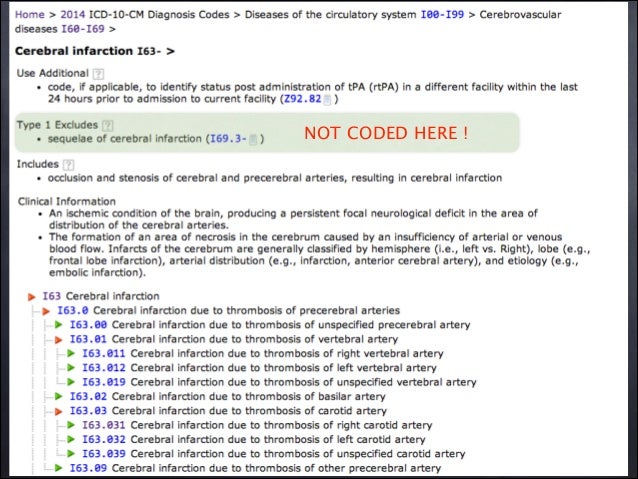
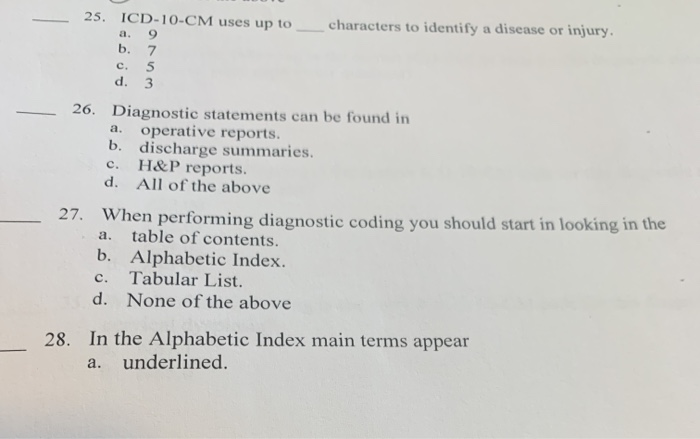
It does not always provide the full code. Alphabetic Index: An alphabetical list of ICD-10-CM (Clinical Modification) terms and their corresponding codes, which helps to determine which section to refer to in the Tabular List.Following is a useful glossary of ICD-10 terms to help ensure a smooth transition. ICD-10-CM Index to Diseases and Injuriesīesides the task of transitioning to ICD-10, surgeons and their staff should become familiar with new terminology to properly code with the expanded code set.ICD-10-CM Tabular List of Diseases and Injuries.For information regarding CDI Boot Camps, click here.
It really would depend on the circumstances of the admission.Įditor’s Note: Sharme Brodie, RN, CCDS, CCDS-O, CDI education specialist and CDI Boot Camp instructor for HCPro in Middleton, Massachusetts, answered this question. There is no rule as to treatment having to be “equal.” Sometimes the provider may determine no treatment (such as medication or surgery) is the best course of action for a patient, maybe monitoring the patient at a different level of care, for instance in the ICU versus placement on a medical/surgical floor is best. To reiterate, first and foremost the selection of the principal diagnosis is based on the circumstances of the admission as stated above, followed by any instructions received in the coding conventions, such as a “code first” note (these instructions or conventions are only found in a code book, you will not find them in the DRG Expert), followed by the advice found in the Official Guidelines for Coding and Reporting, and lastly by any instruction/advice given in the America Hospital Association’s Coding Clinic for ICD-10-CM/PCS published every year on a quarterly bases. It states that “in the unusual instance when two or more diagnoses equally meet the criteria for principal diagnosis as determined by the circumstances of admission, diagnostic workup and/or therapy provided, and the Alphabetic Index, Tabular List, or another coding guidelines does not provide sequencing direction, any one of the diagnoses may be sequenced first.”ĬDI professionals need to read the Official Guidelines for Coding and Reporting, in its entirety, particularly the sections governing principal diagnosis selection. Section II.C., contains rules governing code assignment for two or more conditions that equally meet the definition for principal diagnosis.
The Guidelines further state that “in determining principal diagnosis, coding conventions in the ICD-10-CM, the Tabular List and Alphabetic Index take precedence” over the Guidelines. Furthermore, the Guidelines refer to the rules outlined in CMS’ Uniform Hospital Discharge Data Set (UHDDS) as “that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care.” (The UHDDS definitions are used by hospitals to report inpatient data elements in a standardized manner.) It states that the circumstances of inpatient admission always govern the selection of principal diagnosis. Can you provide the actual verbiage of the coding rule and explain?Ī: The instruction can be found in Section II of the Official Guidelines for Coding and Reporting for Selection of Principal Diagnosis. Q: When two conditions are both present on admission, both meet definition to be the principal diagnosis, and are “equally treated,” my understanding is that the condition does not have to be "equally treated" in the sense of duration/frequency.


 0 kommentar(er)
0 kommentar(er)
